Sleep As Medicine
Health is complicated. Our day-to-day wellbeing and long-term outcomes are determined by many interrelated factors. Some are established, like access to health services. Some we’re just beginning to understand, like the microbiome. Some we’re born with; some we can directly control.
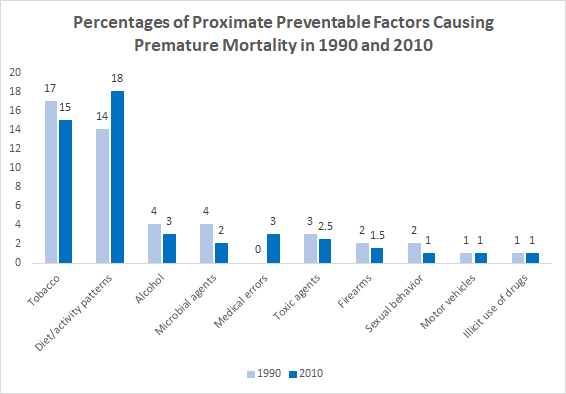
There’s now strong evidence that “lifestyle factors” – behaviors we control and can hope to change – and social determinants account for most premature deaths in the United States. A much smaller percentage (10-15%) could be avoided by better medical care. In other words, most early death is preventable: an individual’s choice to quit smoking and a community’s access to safe places to exercise are subject to change. And we’ve done it before. In the 1990’s tobacco was the leading cause of premature death. It’s since lost the top spot to diet and activity patterns.
Despite evidence that sleep deprivation is a major risk factor for chronic disease, nutrition and exercise have historically gotten most of the attention. These categories are rich with clinical guidance, personal trainers, healthy meal plans, YouTube channels, and more, all ready to help you eat and exercise better. In contrast, it’s almost unbelievable that the best advice for sleep health is to get 8 hours a day. No matter your age, sex, occupation, your sleep goal is typically the same: get 8 hours. Imagine if the best fitness recommendations you could get is to work out 45 minutes a day and limit your calorie intake. No specific information on the benefits of core over cardio, no point of view on whether cutting sugar or fat would be better for cardiac health – nothing else.
Today, the most successful sleep solutions focus on helping you get the right amount of sleep by helping you drift off. It’s obvious that people are willing and even desperate to invest in things that increase the quantity of sleep they get: Ambien and mattresses are big businesses. But these solutions don’t work for many – a third of Americans get less than 7 hours of sleep each night and about 25% experience acute insomnia at some point each year – so new approaches to induce sleep are popping up. Most new solutions aren’t clinical, but some are hugely popular like essential oils and weighted blankets that relax the body and meditation podcasts that quiet a noisy mind.
What happens if these solutions help us fall asleep, but we’re one of the 35%+ of Americans who don’t sleep more than 7 hours each night? Not necessarily because we don’t have the right technology for it, but because there are too many social, economic or even environmental barriers in the way. If we accept that many people will never be able to hit their CDC-recommended 7+ hours each and every night, what opportunities are there to improve sleep quality? How can we make the most of the time that we do have?
Robust research on the mechanisms of sleep remain challenging to conduct at scale, since sleep studies typically require people to spend the night in a lab where their biometrics and brain activity can be measured in person. However, sophisticated diagnostic and tracking devices, which range from wearables (like Onera Health and Oura) to smart beds to apps (like Sleep Cycle and Pillow) that offer insight into time spent in each stage of sleep and number of nightly sleep disturbances – indicators for sleep quality – are coming to market. However, awareness among those who stand to benefit the most from better sleep – people with co-morbid conditions or poor health – remains low. A recent survey showed that while 50%+ of American mobile phone users use mobile technology to track exercise, less than 30% use it to track sleep. Those who consistently measure their sleep are more likely to be both wealthy and healthy. Given the variability of sleeplessness and its correlated factors,at-home tracking tools that allow researchers and individuals to model relationships between daily activities, health conditions, and sleep health across populations, will open up new diagnostic possibilities.
So far we know that if we want to sleep well, we have to give up our unhealthy habits: caffeine after noon, alcohol at night, skipping the gym to binge-watch TV, etc. But the relationship between most other activities and sleep health, especially those positively associated with sleep quality, remains a mystery. And since the context of our lives directly influences our choices, social determinants and behavioral patterns should be considered together when designing interventions that can effectively support healthy sleep habits. As more data comes online, we hope to see more personalized interventions that fit into peoples’ routines.
One source of sleep deterioration is inevitable: old age. As people age they experience more sleep disturbances throughout the night and less time in slow-wave sleep. Moreover, the prevalence of sleep disorders like insomnia and sleep apnea increases with age. There is significant opportunity for interventions that prevent or address declines of sleep quality among older adults.
.png)
You can imagine one day optimizing the natural biology of sleep – brain activity that affects almost every type of tissue and system in the body – to improve other elements of wellbeing. We know that sleep deprivation is a risk factor for a wide range of chronic conditions. But what if sleep is more than a preventive practice?
What if better sleep could treat or reverse related conditions?
One use case could be memory disorders. Using different neurostimulation methods to induce slow wave activity among sleeping individuals, researchers have shown that they can improve memory formation and retention. And now, scientists at Northwestern and Berkeley are testing whether simulating deep sleep (the stage during which memories are formed and encoded) can improve memory and minimize cognitive decline among aging individuals and those with dementia.
Clinical evidence and commercialization for interventions that treat chronic conditions via sleep therapy are a long way’s off. But we’re excited to see the conversation start to expand beyond simple measures of quantity and blunt instruments like Ambien.
When we think of what makes a Collaborative Fund investment, it often comes down to giving people better choices. When it comes to ways to get better sleep, we don’t think we have enough yet - which is why we’re keeping our eyes open for something to fund in the space.
Information sources:
The Case For More Active Policy Attention To Health Promotion J. Michael McGinnis, Pamela Williams-Russo, and James R. Knickman Health Affairs 2002 21:2, 78-93
CDC; Data and Statistics: Short Sleep Duration by Sex, Age, Race/Ethnicity, 2014.
University of Pennsylvania School of Medicine. “One in four Americans develop insomnia each year: 75 percent of those with insomnia recover.” ScienceDaily. ScienceDaily, 5 June 2018.
Rebecca Robbins, Paul Krebs, David M. Rapoport, Girardin Jean-Louis & Dustin T. Duncan (2019)Examining Use of Mobile Phones for Sleep Tracking Among a National Sample in the USA, Health Communication, 34:5, 545-551, DOI: 10.1080/10410236.2017.1422104
Image sources:
Committee on Population; Division of Behavioral and Social Sciences and Education; Board on Health Care Services; National Research Council; Institute of Medicine. Measuring the Risks and Causes of Premature Death: Summary of Workshops. Washington (DC): National Academies Press (US); 2015 Feb 24. 3, Data from Major Studies of Premature Mortality.
Copinschi, Georges and Anne Caufriez. “Sleep and hormonal changes in aging.” Endocrinology and metabolism clinics of North America 42 2 (2013): 371-89 .